According to the Beijing Municipal Bureau of Commerce, in the past May Day holiday, the city’s catering industry implemented the requirements of "suspending in-house meals and switching to take-out services", relying on online ordering, take-out food delivery, and self-help at the store to go all out to protect the lives of citizens during the holiday. Starting from May 5th, the measures of suspending in-house meals and switching to take-away service will continue. In order to further clarify the relevant work requirements, the Municipal Bureau of Commerce has studied and formulated the "Working Guidelines for the Catering Industry during the Suspension of in-house meals".
At present, many high-star hotels and high-end restaurants in Beijing, including Michelin-starred restaurants and Black Pearl restaurants, have launched a variety of takeout. Some high-end restaurants offer cost-effective packages or single-person packages suitable for families and young people; Some have launched family banquet packages full of ceremonies; Others offer prefabricated kebabs and Japanese-style lunches … You can enjoy chef-level roast duck, Buddha jumping wall, clay pot rice and sushi at home without going out.
Roast duck is the most satisfying when you get home, and the price of western-style single package is close to the people.
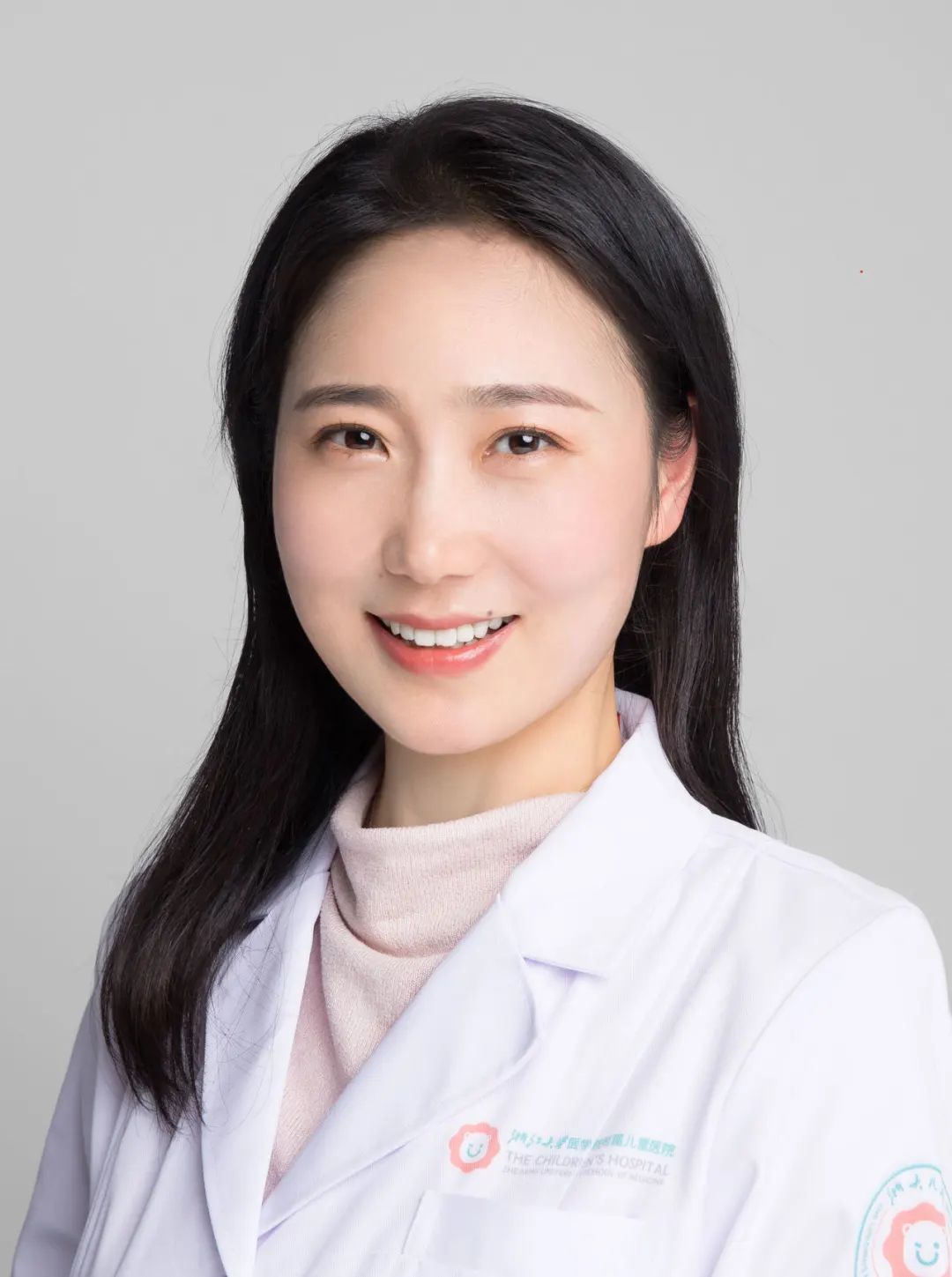
Restaurant: Beijing Kerry Hotel Haitiange and Jiawei.
Order: Hotel WeChat Mall, Meituan, Hungry?
Recommended: roast duck, bacon clay pot rice, western-style single set meal.
Tip: You can send it directly to the hotel within 1 km.
Haitiange Takeaway Package Signature Roast Duck Package.
Beijing Kerry Hotel is rich in take-away dishes, and most of the dishes in Haitiange Restaurant’s food menu can be taken away. In addition, family take-away packages with relatively high sexual prices are specially introduced, including roast duck signature packages, classic Cantonese dishes packages and flavor stir-fried packages, which can be enjoyed by 3-4 people. Jiawei has launched a variety of Western-style packages within 100 yuan, including fried steak, pasta and various salads. Four single-person packages include avocado okra seasonal vegetable salad with honey sesame sauce and grilled salmon fillet with vegetables, which are healthy and delicious, and you don’t have to worry about getting fat at home.
For experienced diners, it’s so happy to eat Master Yuan’s "Beijing Duck Edge" roast duck at home. The roast duck here is very particular. It is said that it has to go through at least 13 processes before entering the oven. Jujube wood is roasted for 70 minutes. When sliced duck, each slice should be willow-leaf-shaped, with a length of 5 cm and a thickness of 0.2 cm. Hand-made duck cake, secret sweet noodle sauce, melon strips, garlic paste and white sugar will be fat but not greasy, and it will melt in the mouth. In addition to half a roast duck, there are also cherry tomatoes, spicy and crisp perch, beef tenderloin with sweet potato and black pepper, prawn-roasted cabbage, fried rice with diced chicken with garlic and asparagus, and yangzhi manna.
Western-style single set meal.
In addition, the classic Cantonese cuisine set meal is recommended, and the traditional bacon clay pot rice is very popular. This dish looks homely, but it is very particular. After washing fragrant rice, put it inbailerBoil the young for 5-10 minutes over medium heat, and collect them.juiceRemove excess starch, and then add Guangdong sausage and bacon together.bailerSimmer for 30-40 minutes, let the rice fully absorb the bacon grease, first season the soy sauce with onion, ginger and garlic, and finally mix withbailerMix well, and the smell is rich.
Modern Sichuan styleIncisively and vividly, the pizza in Rome is healthy and authentic.
Restaurants: Yushe Super Fly, Frasca Italian Restaurant.
Order: Jin Shi Song, Mei Tuan
Recommended: sad fish fillet, Roman Pinsa
Tip: You can pick up and send the bill.
Beijing Yushe’s take-away dishes are very rich.
It is often said that there is no trouble that can’t be solved by a incisive spicy Sichuan dish. The "Super Fly" restaurant in Beijing Yushe is the favorite of many modern young people in Beijing. Even if you can’t go to the dining hall recently, you can take the delicious Sichuan food home. The take-away menu launched by Super Fly, including crispy potatoes, maocai, Sichuan fried noodles, Sichuan braised pork rice, cold noodles with shredded chicken, etc., is mostly less than 100 yuan, and is used as a dish in high-end hotel restaurants.priceQuite close to the people.
In addition to all kinds of Sichuan snacks and staple foods, there are several main courses that can’t be missed, such as sad fish fillets, which are made of fat and tender black fish fillets, boiled in water simply, and finally topped with secret sauce prepared with Sichuan pepper and pepper. The spicy taste is accompanied by fish, which is fresh, tender and smooth and very enjoyable. There is also a pineapple Zuo Zongtang chicken-you know, the most popular Chinese dish in the United States is Zuo Zongtang chicken. The chef innovated and improved this classic dish, adding pineapple to give it a new flavor. The sweet and sour pineapple not only complements the original sweet and sour taste, but also adds the fragrance and crispness of fruit.
Pineapple Zuo Zongtang chicken.
If you want to try exotic food, you might as well order an Italian one.a surname. Hotel Italian restaurantFrascaThe take-away menu is also rich and authentic, especially the classic Italian flavor.Frasca Pinsa”You know, traditional RomePinsaCompared with the public’s familiarityDe pizzaMore healthy. This pizzaCompletely follow Italian recipes,The dough blank is made by mixing Italian wheat flour, soybean flour and rice flour, kneading slowly by hand, adding traditional meat, and baking with firewood and Japanese long charcoal, which tastes authentic.
You can also enjoy the "pot smell" of the clay pot at home, and you don’t have to get off the bus to take the food directly.
Restaurant: Xinmingyuan
Place an order: telephone reservation
Recommended: clay pot series and typhoon shelter series.
Tip: Support self-help drive-in service and flash delivery.
Baked yellow croaker with golden garlic.
Xinmingyuan, which specializes in Cantonese cuisine, has recently launched a take-away menu, including a variety of specialties of chef Xiang Li, such as seafood, signature roast, soup and fresh vegetables. The take-away menu can be a la carte or a set meal, including a set meal for two or four people. You can choose your own vegetarian dishes and staple foods, and you can also give hot and sour soup and vegetarian soup.
Clay pot series is a must-have dish in the take-away menu. Through professional packaging, it retains the "pot smell" and delicacy to the greatest extent. For example, baked yellow croaker with golden garlic, the signature dish, is cooked in a casserole, and the fragrance of carved flowers and garlic cloves is soaked in the fish, which is very tasty. The staple food might as well try the black truffle mushroom sausage chicken pot rice. The chicken is rich in oil, the rice grains are bright in sesame oil, and the bacon is delicate and fragrant, mixed with black truffles, which is extremely delicious. In this takeaway menu, the chef also specially added fresh shrimp balls and boneless pig hands from the typhoon shelter series, which is very suitable for home enjoyment. Of course, don’t miss the restaurant’s signature crispy chicken. Hainan Wenchang chicken skin is thin and smooth, and its color is golden.
Shrimp balls in typhoon shelter.
The take-away service here can not only be delivered by flash, but also provide self-help drive-in service. Before guests arrive at the store, they just need to call the clerk and a specialist will deliver the meal to the car, so they can take the food directly without getting off the bus.
The family banquet is full of sense of ceremony, and professional insulation packaging adds points to Kung Fu dishes.
Restaurant: 1949 whole duck season restaurant
Place an order: telephone reservation, US delegation
Recommended: jujube roast duck, royal Buddha jumping wall
Tip: Pick yourself up, flash.
Slow fire snowflake beef.
Black Pearl Yizuan Restaurant 1949Whole duck seasonThe "Seasonal Food Banquet" was launched, including two packages for 2-3 people and 4-6 people. Among them, 40-year-old jujube roast duck, Huajiao Zhanjiang chicken, beef tenderloin with black pepper, and spring bamboo shoots braised with cherry shrimp oil are all signature dishes of the Executive Chef, so that you can get a full sense of ceremony at home.
Roast duck is the first choice. The selection of materials and the baking method strictly follow the ancient method. Jujube wood over 40 years old is selected, baked in the oven, and baked on time in 65 minutes. It is very delicious with original duck sauce. In addition, slow-fire snowflake beef, asparagus fried scallops and the Royal Buddha Leaping Wall are all very suitable for take-out. Among them, the Royal Buddha Leaping Wall is personally managed by the executive chef, including eight fresh abalone, Kanto ginseng, scallop, skirt, gelatin belly, Tricholoma matsutake and other ingredients. It is golden and bright, and the juice is thick and thick. It is still warm when it is packed in a professional insulated take-out bag.
Fried scallop with asparagus.
Snowflake beef with slow fire is a time-consuming and laborious kung fu dish. Snowflake beef is the main ingredient, and it is boiled for 2 hours with slow fire, and then the secret beef soup is added. The meat is fragrant and melts in the mouth. Stir-fried scallops with asparagus are very demanding on ingredients. Considering the chef’s cooking skills, it is necessary to choose fresh scallops with specifications of 6 Liang each.Yuanbei, limited sales of 120 a day, huge and full of fresh.YuanbeiWith asparagus, it is crystal clear. In addition, the takeaway menu also has spicy duck gizzards.Toona sinensis fresh walnut kernel, green tofu duck soupWaiting for more than 30 orders.
Japanese skewers are prefabricated in advance, and dried puffer fish with wine is particularly pleasant.
Restaurant: ITO Ito
Place an order: telephone reservation
Recommended: BBQ set meal
Tip: Support self-help drive-in service and flash delivery.
Barbecue set meal.
Japanese restaurant ITO Ito’s takeaway menu is served by the chef.KalokPersonal design can bring unexpected little surprises to home life. The takeaway menu is very rich, includingburnFood, vegetables, seafood, etc. The best thing is the barbecue set meal-prefabrication.skewer, suitable for 2-3 people, including restaurant signs.Baked goodsBeef ribs, beef tongue with salt onion, roasted bird with long onion, etc. The chef will put it in advanceskewerThe ingredients are marinated, and the taste is restored to the maximum extent. Just put them in the oven at home. With fresh salad, edamame, and a bottle of sake, it is especially pleasant to have a drink at night.
Specially served eel rice.
Dried puffer fish is especially recommended for side dishes with wine. It is tender and delicious.Full, you can eat a plate before you know it. In addition,Salt roastingredtigerShrimp meat is full,Braised eel puSoaked with juice, oiljuiceBlended with sauce, it is full and delicious, and it is the best partner for drinking. Finally, don’t forget to order a special eel rice. As Ito’s signature, the chef uses a whole eel to let you experience three ingenious ways to eat it: enjoy it wrapped directly.secretFlavor the sauce.glutinousEel rice; Or add small materials to match a richer level; Or put bonito juicewaterFinish the eel rice, and use the lightness of the soup to "neutralize" the thickness of the eel.
The six-course set meal gives consideration to nutrition and flavor, and English afternoon tea brings good afternoon time.
Restaurant: Huangting and Lobby Teahouse of Wangfu Peninsula Hotel.
Place an order: Official WeChat Mall
Recommended: Six-course family set meal, English afternoon tea.
Tip: Take it yourself.
HuangtingChinese restaurant six-course family package.
Wangfu Peninsula Hotel has launched quick take-away service, including six-course family package in Huangting Chinese restaurant and classic English afternoon tea in the teahouse in Peninsula lobby. Among them, the Huangting six-course take-away family package was designed by chef Shi Chenrong himself. He always pays attention to the freshness and origin of ingredients, and combines the classic Cantonese cooking techniques and the characteristics of Jiangnan cuisine to make the dishes richer and healthier. The six take-away dishes include rose fried chicken with black bean sauce, steamed yellow croaker with dried tangerine peel and black bean sauce, stewed beef brisket with Morchella and silver radish, crispy shrimp with fresh mushrooms, fried rice with celery fragrance and scallop protein beside the cloud ears, etc., which are rich and mellow, or crisp and tender, paying attention to flavor collocation and health. For example, a stew of beef brisket with Morchella and silver radish, beef brisket with seasonal vegetables, using the slow cooking skills in traditional Cantonese cuisine, preserved the original flavor of beef brisket and Morchella.

English afternoon tea.
Classic English afternoon tea is the signature of Peninsula Hotel. The take-away afternoon tea package launched by the lobby teahouse of Wangfu Peninsula Hotel includes selected sandwiches, hand-made desserts and freshly baked Si Kang every day. The take-away afternoon tea gift box is also very exquisite. The top layer is four exquisite desserts: mint cream cheese mango roll, pistachio hazelnut Mu Si, vanilla cream strawberry tower and strawberry cream cake. The middle layer is salty, including foie gras black truffle tower, smoked salmon sandwich, sweet shrimp and egg sandwich, herb salad cucumber sandwich; The lower floor is the classic original flavor of the peninsula and raisin scones, with traditional condensed cream and homemade vanilla cream raspberry jam, so that you can have a leisurely afternoon at home.
Sakura bento is exquisite, creating a picnic and camping atmosphere at home.
Restaurant: Four Leaf Sushi
Place an order: telephone reservation
Recommended: cherry blossom heavy box diet
Tip: Support self-collection, free flash within 10 kilometers, it is recommended to book at least 2 hours in advance.
Sakura heavy box meal.
If you want something romantic and create the feeling of picnic and camping at home, you might as well try exquisite Japanese bento. Four-leaf sushi is an old-fashioned high-end Japanese food in Beijing, and its Lido store, Zhongguancun store, Sanlitun store and Yansha store have recently launched a limited takeaway lunch-cherry blossom heavy box meal. According to reports, the dining box is a traditional small wooden box in Japan, mostly rectangular or square, which is usually used to put tableware, and the lid can be used as a small dining table when eating. Four leaves use exquisite cherry blossom three-layer dining box, and the outer layer is wrapped with wind decorative cloth, which is very eye-catching. After eating, the dining box can be kept for yourself and used as tableware for picnic and camping.
The lunch box set is rich in dishes.
The signature of four-leaf sushi is "Japanese traditional hand-held sushi", which is very particular about both raw materials and cooking techniques. The content of this takeaway package is also quite rich. The four stores are different, including eel package and fried rice package. Among them, four-leaf Zhongguancun store’s three limited packages-early summer eel package, seafood eight-fold package and luxury seafood assorted sushi package, are composed of appetizer, boiled food, roasted food and staple food, respectively, and packed into three-tier boxes, which are exquisitely matched and balanced in nutrition. It is recommended that the seafood eight-fold too-roll package includes naked bluefin tuna, bamboo pod fish, tuna thin roll, Japanese salted radish, egg roll, etc., which is full of happiness.
The sumptuous seafood assorted sushi set includes five kinds of sashimi platters, boiled small conch, crab leg with pine leaves, Iberian black pork asparagus rolls, etc., as well as the sumptuous assorted sushi as the staple food, which is made of bluefin tuna mud, sea urchin, salmon roe, sturgeon roe, scallop, salmon roe, egg roll, crab roe, etc., and sushi rice, and each bite is extremely delicious.
Enjoy the famous dishes of state banquet at home, such as Buddha jumping over the wall, boiled cabbage,Zhangcha duck is a classic.
Restaurant: the ginseng
Place an order: order by phone
Recommended: Buddha jumps over the wall and boiled cabbage.
Tip: Pick yourself up, flash.
Buddha jumps over the wall.
If you want to enjoy the authentic national banquet dishes at home, you may wish to know about it.joinThe take-away menu in the restaurant. This Michelin bibendum restaurant, located in the front door, specializes in state banquet dishes, and retains the dishes of Beijing Hotel, such as Lohan’s belly, General Chen’s chicken, sea cucumber with onion, lion’s head with crab powder and boiled cabbage. According to reports, at present, all the dishes in the restaurant can be packaged to provide take-away service.
Boiled cabbage.
This means that you can also eat the classic Buddha jumping wall at home. You know, there are many ways to cook this traditional famous dish, but the ginseng restaurant uses the traditional method-stewed abalone, Liaoshen, gelatin, deer tendon, ham, old chicken, old duck, mushroom, sheep’s hoof, pork belly, scallop and other ingredients used in boiled cabbage. The highlight of this dish is that it fully reflects the taste and characteristics of each ingredient. Therefore, it is necessary to make these dozens of ingredients into a dish independently, and then gather together, add "clear soup" and simmer for several hours. The soup is clear and strong.
Another Zhangcha duck, with crispy skin and crisp meat, is also very suitable for eating at home. This dish is fastidious. Ducks are cooked by pickling, smoking, steaming and frying, and the smoking time is especially strict. There are six or seven kinds of smoking materials, including fine tea, pine and cypress branches and brown sugar.
The dishes and ingredients are delivered home in order to experience the good flavor of Qilu.
Restaurant: Lucai
Place an order: telephone reservation
Recommended: Raw juice sea cucumber soup, home worry-free four-pack and so on.
Tip: Pick it up or deliver it. Employees of Nei Lu Mining Company will deliver it in person within 5km, and flash delivery can be made outside 5km.
Raw juice sea cucumber soup.
RuceFeaturing all kinds of Jiaodong seafood, supplemented by jinan cuisine and Confucius dishes, it is a representative restaurant of the new Shandong cuisine in the hearts of many diners. Recently,RuceA variety of take-away services have been launched, including "Worry-Free at Home" in addition to dishes.bagIngredients and prepared dishes. Takeaway dishes include cold dishes,Pasta, hot dishes, etc., such ashot spice plantMa seafood, prawns in Bohai Bay, roasted cabbage and sand.Cattle tendonWait. "worry-free home" four companiesbagIt is delivered on a fixed day every week. In addition to the finished dishes, there are many kinds of fresh and vegetables, such as prawns, pig hands, Toona sinensis, clams and black-bone chickens.
Donkey gum nourishing black garlic soup.
You can also order some specialty dishes of the restaurant, such as raw sea cucumber soup. Choose wild sea cucumbers over 5 years old, and make sure that the nutrition is not lost. Only add salt and pepper in the cooking process. Interestingly, the sea cucumber soup is green. It is said that the original soup is green because wild sea cucumbers eat natural seaweed. There is also a soup with donkey glue nourishing black garlic, which also has a typical Qilu flavor. After simmering donkey glue and donkey meat for more than ten hours, add black garlic and steam it for four hours, so that the nutrition of donkey glue, donkey meat and black garlic can be completely dissolved in the soup, and the entrance is slightly sticky and very sweet.
Afternoon tea and dessert bring sweetness, and Mother’s Day gives mom a surprise.
Restaurants: Beijing Bulgari Hotel, The Ritz-Carlton Beijing Financial Street, Beijing Magnificent Hotel.
Place an order: telephone reservation, WeChat mall, etc.
Recommended: afternoon tea and dessert.
Tip: Pick yourself up, flash.
For a delicate girl, how can there be no afternoon tea and dessert in the spring? Many high-star hotels, such as Beijing Bulgari Hotel, Beijing Magnificent Hotel and The Ritz-Carlton Hotel in Beijing Financial Street, have launched afternoon tea or dessert take-away service, and you can also enjoy sunshine, dessert and happiness at home. It’s Mother’s Day this weekend, so it’s good to give my mother a surprise.
Italian raspberry fruit tower.
It is recommended to try the "La Pasticceria-Niko Romito" Italian dessert in Beijing Bulgari Hotel, which is a series of cakes created by Michelin-starred chef Nico Romito, including 11 kinds, all inspired by traditional Italian recipes, and reduced the use of animal fat and sugar in the production process, making it healthier. After purchase, the hotel can provide Bulgari packaging boxes for easy take-out.
Bulgari white chocolate rose raspberry cake.
In addition, the appearance of each pastry is also the "ceiling" of dessert aesthetics, and every detail is full of beauty. Among them, the Italian raspberry fruit tower and chocolate puffs are very popular classic delicacies. Bulgari’s hand-made cake is also worth trying, with fresh ingredients and elegant colors, including eight flavors: golden toffee, peach blossom tea, Italian cappuccino, berry pistachio, hazelnut chocolate, strawberry chocolate, chocolate raspberry and white chocolate rose raspberry.
Mother’s day afternoon tea gift box.
The Magnificent Hotel in Beijing has launched the take-away service of customized afternoon tea and limited cakes for Mother’s Day. Among them, Qindie Mother’s Day afternoon tea includes daily freshly baked cakes, tea-scented sandwiches, signature strawberry and vanilla thousand-layer cakes and a variety of Mother’s Day limited desserts, which are very exquisite. In addition, there are a variety of cakes that are also suitable for giving to mothers. Among them, strawberry Qifeng cake is very sweet with dense Hokkaido cream and strawberries in season. Cherry Charlotte cake is made up of finger cakes and fresh cherries, which is very cute; Limited vanilla strawberry Melaleuca cake adds a touch of sweetness to May.
Takeaway cake
The Ritz-Carlton Beijing Financial Street not only provides exquisite afternoon tea take-out, but also provides cakes with various flavors such as French strawberries, black forest, white chocolate and citrus sandwich, western-style dim sum series and crispy beef patties in old Beijing, so that you can have a wonderful afternoon.
Beijing News Shell Financial Reporter Qu Xiaoyi
Editor Jake
Proofread Liu Baoqing
Photo interviewee provides